First, we went over what medical problem would lead to this procedure -- leukemia, which is cancer of the white blood cells. Normally, white blood cells are part of our immune system, so they protect us from infections. In leukemia, some type of white blood cell is reproducing out of control and often isn't performing its protective job. You can see under the microscope that there are way too many of a certain type of cell. The symptoms of leukemia include fatigue (tiredness), bruising, bleeding, pallor (Pale skin), enlarged organs, and infections. When a patient first has leukemia, they are usually treated with chemotherapy, which is drug treatments that are supposed to kill off the cancer cells.
Side effects of chemotherapy include losing your hair, because the drugs kill off cells in our body that are dividing and reproducing rapidly. Hair follicle cells divide frequently, so the cancer drugs kill those cells, resulting in hair loss. People also get mouth ulcers, fell nauseous and have diarrhea, as well as changes in their blood from chemotherapy. Our patients in the game had done chemotherapy first and their disease went into remission. That means their symptoms went away and it seemed like the cancer was gone. But somehow a cancer cell must have been missed and the leukemia came back. That's called a relapse, and it means a new treatment is needed. That's why they might have a stem cell transplant.
The idea is that to get rid of the cancer of the blood cells, you can try killing off all of the patient's bone marrow stem cells (where the cancer cells are living and hiding out), which are the cells that make the blood cells. Then, you transplant stem cells from someone who doesn't have leukemia, and the patient can then grow a whole new immune system that doesn't have cancer. It's VERY risky, and that's why chemotherapy is always first. Only if chemotherapy doesn't work do they try this procedure. Here are the main risks of the stem cell transplant procedure:
- The drugs they use to kill off the cancer and the patient's bone marrow cells could make the patient extremely sick
- When the patient has no bone marrow stem cells, they have no immune system, so any little infection could kill them
- They could reject the new cells and be left with no immune system, which is very dangerous
- The new immune system could reject them, and attack their healthy cells. This is called Graft Versus Host Disease, and it's dangerous and uncomfortable.
 We walked through all the steps involved in the procedure. The first thing to do is to confirm that that patient's cancer has returned. We looked at slides of the patients' blood to see if there are cancer cells in the blood. The larger cells in these pictures were the cancer cells. Both of our patients had cancer cells in their blood, and that's how it was decided that they needed a stem cell transplant.
We walked through all the steps involved in the procedure. The first thing to do is to confirm that that patient's cancer has returned. We looked at slides of the patients' blood to see if there are cancer cells in the blood. The larger cells in these pictures were the cancer cells. Both of our patients had cancer cells in their blood, and that's how it was decided that they needed a stem cell transplant.Next, we actually learned a bit about our patients, Wendy and Michael. Wendy, our first patient, is a high school student who developed leukemia her freshman year and got better with chemotherapy. But a year later, the cancer is back. She has read all the information about the procedure and understands all the risks. She wants to know if everything will be done in time for her to go to her junior prom. The doctor says she'll do everything she can to have Wendy well in the next six months, so she can go to the dance.
The next step is to find a donor -- a person who is willing to give their bone marrow stem cells to the patient. The first thing we do is check full siblings, then close relatives, and then a list of people willing to donate their bone marrow (the registry). There are 8 million registered donors, but most of them are caucasian (white). So Wendy's chance is 66% of finding a donor. Unfortunately, an African American has less than a 25% chance of finding a donor, and a Hispanic/Latino patient has about a 5% chance.
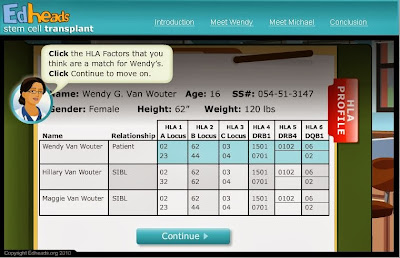
What you're looking for in choosing a donor is something called HLA, Human Leukocyte Antigen.
People have 6 markers on our cells that tell the immune system whether the cells are foreign or part of our own bodies. It needs to be a pretty good match to avoid the graft attacking the patient's own body because it thinks the cells are foreign. We looked at all 6 HLAs for Wendy and her two sisters, hoping that one is at least a match for 5 out of 6. In fact, her sister Hillary is a match for 5/6 and her sister Maggie is a match for all 6, so Maggie is the best donor.
Conditioning is the procedure of using drugs and radiation to kill off the leukemia and the bone marrow stem cells. Wendy has to stay in the hospital with special air flow conditions to keep germs and bacteria away from her while she has no immune system. At the right time, Maggie is given drugs that make the bone marrow stem cells go into the blood, and then her blood is collected to gather the stem cells to transplant.
The cells are put into Wendy's body through her central line, right into her blood. She stays in the protective area in the hospital, and the doctors keep checking her blood to see when she has enough of an immune system to go home. We counted neutrophils on this slide to see if she has at least 500 neutrophils per microliter. She did, so now she can go home, if her temperature and blood pressure are ok. She has a fever, so she has to stay in the hospital until it's gone. 3 days later, she's fine and can go home. 3 weeks later, her transplant still seems to be ok, but she has a rash all over, diarrhea, and is swollen. It's Graft Versus Host Disease, her new immune system is attacking various parts of her body. She has to come back into the hospital and go onto steroids, which reduce the swelling and diarrhea, but she still has some symptoms. They decide to do an experimental procedure that might help with her symptoms. They don't know that it will work, don't know what side effects might happen, and it might cause an allergic reaction or some other problem. She decides to try the experimental therapy, and it works. I pointed out that this part is not necessarily realistic. Experimental treatments do not always work. In fact, most of the time they don't work, but it's important to try them because that helps us learn more so we can find treatments that do work.
We moved on to the next patient, Michael, who has the same disease but a different situation. He is an older, African American gentleman, and he cannot find a suitable donor. So, he has a cord blood stem cell transplant, which is when they take stem cells from the umbilical cord of a newborn baby that have been stored and use them for the transplant. It often takes longer for the new immune system to start working. I encourage you to explore this part of the game.